Can a PA be a primary care provider?
Yes, of course!
As our healthcare system evolves and grows, the demand for primary care providers has increased.
Today, physician assistants are increasingly filling the demand in primary care.
The Senior Soup delves into the role that a primary care physician assistant plays and explores how they can effectively serve as family practitioners and even help underserved populations and older adults under the supervision of a physician.
Bottom Line: Can a PA be a primary care provider?
Yes, a PA can be a primary care provider!
A physician assistant (PA) is a licensed healthcare professional who practices medicine under the supervision of a physician.
They work in various healthcare settings and specialties, collaborating with physicians and other healthcare clinicians to deliver comprehensive and efficient patient care.
More and more physician assistants today are serving as primary care providers.
Physician assistants: Definition and scope of practice as primary providers
The scope of practice for a PA may vary depending on the hospital, jurisdiction, and the level of physician supervision, but they typically perform the following primary care services:
- Conducting physical exams;
- Diagnosing and treating illnesses;
- Performing preventive care;
- Ordering and interpreting diagnostic tests;
- Writing prescriptions;
- Performing medical procedures;
- Providing patient education and counseling.
What educational credentials are required to become a physician assistant?
Physician assistants must do the following to become licensed healthcare clinicians:
- Complete a series of educational and certification requirements;
- Earn a bachelor’s degree;
- Graduate from an accredited physician assistant program;
- Obtain certification and state licensure;
- Engage in ongoing continuing medical education and recertifications to maintain their credentials to practice medicine under a supervising physician.
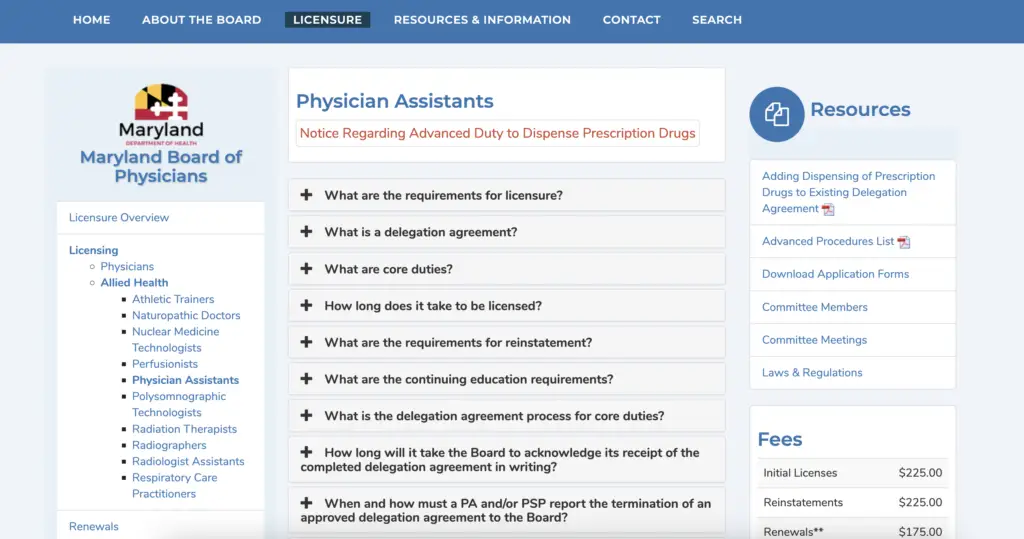
Visit the Maryland Board of Physicians website to understand the licensure process for physician assistants practicing in Maryland.
Required physician assistant educational credentials
Earn a bachelor’s degree.
Aspiring PAs must first complete a bachelor’s degree, typically in a science-related field, such as biology, chemistry, or health sciences.
Some PA programs also require applicants to complete specific prerequisite coursework in anatomy, physiology, microbiology, and statistics.
Graduate from an accredited physician assistant program
A PA must complete a bachelor’s degree, graduate from an accredited PA program, obtain certification and state licensure, and engage in ongoing continuing medical education and recertification to maintain their credentials and practice in the field.
Physician Assistant candidates must complete an accredited educational program, which typically takes two or three years.

Similar to medical school, these educational programs are designed to provide both classroom instruction and clinical rotations, covering subjects such as medical ethics, pharmacology, clinical medicine, and physical diagnosis.
During their clinical rotations, PA students also gain hands-on experience in various medical specialties, such as family medicine within a family practice, internal medicine, pediatrics, and emergency medicine.
Certification
Once a physician assistant student graduates from PA school, completing their physician assistant studies, they must pass a certification exam to become a certified physician assistant.
In the United States, the certifying body is the National Commission on Certification of Physician Assistants (NCCPA), which administers the Physician Assistant National Certifying Exam (PANCE).
After passing the PANCE, graduates earn the title “Physician Assistant-Certified” (PA-C) and begin practicing medicine under a
State licensure
Physician assistants must also obtain medical licensure in the state or jurisdiction where they plan to practice medicine.
Licensing requirements vary by location and typically include the following:
- Completing an accredited physician assistant program;
- Passing a certification exam;
- Then, the PA school graduate must apply to the appropriate state licensing board.
Continuing medical education (CME) and recertification
PAs must complete ongoing continuing medical education (CME) and pass periodic recertification exams to maintain their certification and licensure.
In the United States, PAs must complete recertification every ten years by passing the Physician Assistant National Recertifying Exam (PANRE) and completing one hundred CME hours every two years.
What is the difference between a physician assistant and a doctor?
The primary difference between a physician assistant and a medical doctor lies in their education, training, and scope of practice.
A medical doctor completes a longer and more specialized education and training process, including medical school and residency. In contrast, PAs complete a shorter, more generalized education in a physician assistant program.
Doctors have a broader and more independent practice scope.
At the same time, a physician assistant works under the supervision of a physician and has a more limited range of practice, which can vary depending on the jurisdiction and level of supervision.
Have you been thinking about breaking up with your current doctor?
Do not fear!
The Senior Soup wrote a comprehensive guide on how to break up with your doctor (and find a new one).
Can physician assistants prescribe medications?
Yes, physician assistants (and nurse practitioners) are generally authorized to prescribe medications, although the specific prescribing authority may vary depending on the jurisdiction and the level of doctor supervision.
In some cases, primary care PAs may be required to have a collaborative practice agreement with a supervising physician that outlines the drugs they can prescribe and any limitations on their prescribing authority.
What types of healthcare settings do physician assistants work in?
Physician assistants work as healthcare providers within a wide range of healthcare settings, including, but not limited to:
- Primary care officers, under supervisory primary care doctors;
- Hospitals;
- An emergency room;
- Outpatient facilities;
- Long-term care facilities;
- Specialty clinics.
- Academia and research;
- Psychiatry;
- Neurology.
PAs also practice in various medical verticles, such as family medicine, general internal medicine, public health, pediatrics, emergency medicine, dermatology, surgery, women’s health, and plastic surgery or medical health spas.

What’s the difference between a physician assistant and a nurse practitioner?
Physician assistants (PAs) and nurse practitioners (NPs) are essential healthcare clinicians who play significant roles in providing primary care to older adults.
While they share the same duties and some similarities, there are critical differences between the two professions.
Education and training
PAs complete a bachelor’s degree, typically in a science-related field, followed by an accredited educational program, which takes about two to three years.
These programs provide classroom instruction and clinical rotations, focusing on general medicine and various medical specialties.
Nurse practitioners are registered nurses (RNs) who have obtained a master’s or doctoral degree in nursing, typically focusing on a specific patient population or area of practice.
NP programs emphasize nursing theory, advanced practice nursing skills, and specialized knowledge in their chosen area of expertise.
Licensing and certification
PAs and NPs must be licensed and certified to practice in their respective fields.
Nurse practitioners are certified by nursing organizations, such as the American Nurses Credentialing Center (ANCC) or the American Academy of Nurse Practitioners Certification Board (AANPCB), depending on their specialty.
Scope of practice
The scope of practice for PAs and NPs can vary depending on the jurisdiction and healthcare setting.
Generally, physician assistants work under the supervision of a physician and have a more generalized scope of practice, allowing them to work in various medical specialties.
On the other hand, nurse practitioners often have a more technical scope of practice focused on their chosen patient population or area of expertise.
In many jurisdictions, NPs have greater autonomy and can practice independently without the supervision of a physician, although this can vary depending on the regulations in place.

Why are physician assistants critically crucial to our healthcare process?
Physician assistants are critical to our healthcare process because they can or are:
- Address physician shortages as primary care providers;
- Help improve cost-effectiveness in our healthcare system;
- Practice team-based primary care;
- Flexible and adaptable;
- Ensure continuity of care, notably as primary care providers;
- Educate their patients on preventive health measures and healthier living;
- Provide access to healthcare or serve as a primary care provider in rural communities throughout the U.S.
Keep reading to learn more!
Addressing physician shortages in primary care
The demand for primary care services in the United States is rising due to an older adult population and an increased prevalence of chronic diseases.
PAs help address the shortage of primary care physicians by extending the reach of healthcare services and patient care providers while offering timely and accessible care.
They improve cost-effectiveness in our healthcare system
PAs provide high-quality health services at a lower cost than physicians, which can help reduce healthcare costs for patients and the overall healthcare system.
By utilizing PAs in primary care, resources can be allocated more efficiently, ensuring patients receive the care they need without overburdening the system.
Team-based patient care
Physician assistants are trained to work as part of a collaborative healthcare team, essential in primary care settings.
They work closely with physicians, nurses, and other healthcare providers within clinical practice to provide comprehensive, coordinated patient care, improving overall health outcomes.
Flexibility and adaptability
PAs have a broad scope of practice, allowing them to adapt to various healthcare settings and patient needs.
This versatility enables physician assistants to work collaboratively under the supervision of a primary care physician and offer the following medical services:
- Preventive care;
- Disease prevention;
- Acute illness treatment;
- Ongoing treatment plans;
- Minor procedures;
- Chronic disease management.
Continuity of care
PAs often build close relationships with their patients, fostering trust and lasting rapport.
Continuity of care is crucial in primary care settings, where patients often require ongoing management and follow-up for various health conditions.
PAs help ensure that patients receive consistent, high-quality primary care over time.
Patient education and counseling
PAs are vital in educating our aging population about their health conditions, conducting physical exams, and providing various treatment options.
They also guide lifestyle changes and self-management strategies, empowering patients to take active healthcare roles.
Access to care in rural and underserved areas
PAs can help bridge the gap in primary care access for populations in rural and underserved areas.
They contribute to reducing health disparities and improving overall population health by providing care in remote communities throughout the U.S. where medical doctors do not have an established medical practice.

What are the benefits of a primary care physician assistant?
There are several advantages to having a physician assistant as your primary care provider.
Access to care
PAs can help address the shortage of primary care physicians, making it easier for patients to receive timely and accessible care.
Cost-effectiveness
They can provide high-quality care at a lower cost than physicians, potentially reducing healthcare costs for patients and the healthcare system.
Continuity of care
They can develop long-term relationships with patients and provide consistent care, improving health outcomes.
Team-based care
They often work alongside physicians and other healthcare professionals, facilitating a collaborative and coordinated approach to primary care.
So, can a PA be a primary care provider? Yes!
Physician Assistants (PAs) can serve as primary care providers in many healthcare settings, including home-based primary care!
With their advanced education, clinical skills, and ability to work autonomously or collaborate with physicians, PAs have proven invaluable assets in addressing the growing demand for primary care services.
As healthcare systems evolve and adapt to the needs of diverse patient populations, the role of PAs as primary care providers will only become more significant.
To ensure that PAs can continue to provide high-quality, accessible care, patients, healthcare professionals, and policymakers need to advocate for expanding their scope of practice, increased recognition, and ongoing professional development opportunities.
We can build a more robust, inclusive, and efficient primary care system for all.
Ryan Miner, MBA | Co-Founder and Podcast Host | The Senior Soup
Ryan Miner and Raquel Micit are the co-founders of The Senior Soup and host The Senior Soup Post. Raquel and Ryan have over 25 years of combined experience in the healthcare, medical and pharmaceutical industries.
- The Senior Soup | Raquel Micit & Ryan Minerhttps://theseniorsoup.com/author/raquelryan2/
- The Senior Soup | Raquel Micit & Ryan Minerhttps://theseniorsoup.com/author/raquelryan2/
- The Senior Soup | Raquel Micit & Ryan Minerhttps://theseniorsoup.com/author/raquelryan2/
- The Senior Soup | Raquel Micit & Ryan Minerhttps://theseniorsoup.com/author/raquelryan2/