In the dynamic landscape of healthcare, understanding the roles of nurse practitioners and physician assistants in primary care is crucial.
Older adults have frequently shared their misconceptions and reservations about receiving primary care services from nurse practitioners and physician assistants rather than medical doctors.
The most common misconception I hear about nurse practitioners and physician assistants is that they are less qualified to practice primary care than medical doctors.
I could not disagree more.
I want to address older adults’ concerns about NPs and PAs by highlighting their extensive clinical training and proven efficacy in delivering compassionate, safe, and comprehensive primary care.

In my professional healthcare marketing role with Ennoble Care, I have worked alongside several outstanding nurse practitioners and physician assistants who consistently offer their patients unparalleled, high-quality, and personalized home-based primary care.
This article will feature a comprehensive list of research studies demonstrating the high-quality healthcare services that nurse practitioners and physician assistants provide to their older adult patients.
Each study is carefully selected for its legitimacy, credibility, and rigorous methodology and is well sourced from peer-reviewed journals, reputable medical organizations, and leading healthcare researchers.
Alright, let’s dig in!
Nurse Practitioners and Physician Assistants in Primary Care
It’s natural to want the best primary care possible.
However, it’s critical to understand who provides your primary care and how well they are equipped to do so.
I want to address some common concerns and misconceptions and clarify nurse practitioners’ and physician assistants’ qualifications and capabilities in a primary care context.
First, I’ll dive into nurse practitioners’ roles in primary care, followed by physician assistants’ roles.
The Evolution of American Primary Care: Embracing Nurse Practitioners and Physician Assistants
Our American primary care landscape has undergone significant transformations over the past few decades, driven by factors such as an aging population and a growing emphasis on preventive care.
As documented by The Commonwealth Fund, many patients now face challenges accessing primary care physicians.
This shift, driven by the growing need for accessible and efficient healthcare, shows a broader acceptance and integration of nurse practitioners and physician assistants in primary care.
Understanding these changes helps clarify why seeing an NP or PA for primary care has become increasingly common, particularly for older adults.
Nurse Practitioners and Physician Assistants Expand Access to Primary Care
According to American Medical Association President Jesse M. Ehrenfeld, M.D., primary care in the U.S. is facing provider shortages, especially in rural and underserved areas.
With the growing aging population and the demand for healthcare services, the traditional model of relying solely on physicians (MDs) has proven insufficient to meet these ever-increasing primary care needs.
NPs and PAs are critically essential in bridging the healthcare gap.

These clinicians’ advanced medical training empowers them to provide comprehensive primary care services to older adults, from managing chronic diseases to providing palliative care and pain symptom management.
Most importantly, physician assistants and nurse practitioners help expand access to healthcare for communities that might otherwise face significant provider shortages.
Educational Advancements and Legislative Support for Nurse Practitioners and Physician Assistants in Primary Care
According to the American Academy of Family Physicians, the educational frameworks for NPs and PAs have evolved to prepare them for primary care settings thoroughly.
Nurse practitioners are educated in graduate-level nursing programs that focus on patient-centered care. In contrast, physician assistants complete master’s degrees in accredited PA programs and receive training in medical science that focuses on providing supervised medical care.

Both physician assistants and nurse practitioners must complete extensive clinical rotations that provide direct patient care experience, similar to medical doctors.
Over time, state legislatures and medical boards have expanded the scope of practice for these medical professionals, allowing them more autonomy in diagnosing diseases, managing treatment plans, and prescribing medications.
Cost-Effective Integration of Nurse Practitioners and Physician Assistants in Primary Care Teams
Integrating NPs and PAs into American primary care teams has proven immensely cost-effective for our national healthcare system.
In a large national sample of Americans with complex medical conditions, including diabetes, a study found that physicians (medical doctors) have:
- Higher rates of hospitalizations;
- More emergency department visits;
- Increased healthcare costs.
This data was compared to patients who see nurse practitioners or physician assistants, even after accounting for meaningful patient and facility factors.
These findings are significant because the study compared nurse practitioners and physician assistants in primary care roles similar to those of physicians, and it assessed the total cost of care over one year.
The study found that nurse practitioners and physician assistants provide cost-efficient care without compromising patient satisfaction or outcomes.

NPs and PAs can spend more time with patients during each visit, focusing on education and preventive care. This approach can significantly improve health outcomes, particularly in managing chronic conditions common among older adults.
For more detailed insights, please review the 2019 study by Donelan et al. published in Health Affairs, titled Impact of Physicians, Nurse Practitioners, and Physician Assistants on Utilization and Costs for Complex Patients.
High Patient Satisfaction and Improved Healthcare Outcomes with Nurse Practitioners and Physician Assistants
Patients treated by nurse practitioners and physician assistants often report high satisfaction with their care, citing the providers’ holistic and attentive approach.
Studies by Eriksson, Lindblad, Möller, and Gillsjö (2017) and Roblin, Becker, Adams, Howard, and Roberts (2004) support this positive perception.
Research suggests that the patient-centered model practiced by NPs and PAs may lead to fewer hospitalizations, reduced healthcare costs, and better management of chronic diseases, including a study by Mileski, Pannu, Payne, Sterling, and McClay (2020).
This could be due to factors such as the focus on preventative care and the emphasis on building strong patient relationships.

Consistency of care and strong relationships between patients and their NPs or PAs can significantly enhance patient engagement and health monitoring.
For instance, patients might be more likely to adhere to medication schedules or preventative care recommendations when they have a trusted provider they feel comfortable talking to.
Team-Based Care: The Vital Role of NPs and PAs in Collaborative Primary Care
The shift toward team-based primary care has further solidified the role of NPs and PAs in primary care.
This model emphasizes collaboration among healthcare professionals, including physicians, nurses, behavioral health specialists, specialist providers, and many others, to provide the most comprehensive care possible.

In this setting, NPs and PAs are vital team members who contribute to and often lead patient care management. This collaborative approach leverages each team member’s strengths and skills, enhancing patient care and system efficiency.
Addressing Hesitations and Biases Toward Nurse Practitioners and Physician Assistants Among Older Adults
Older adults may hesitate or resist seeing nurse practitioners and physician assistants for primary care, often preferring medical doctors.
Still, many older adults have difficulty articulating specific reasons for not wanting to see NPs and PAs beyond their preconceived assumptions. Their reluctance to see them may stem from a lack of understanding of their extensive education and clinical training.

Understanding and Overcoming Preconceived Biases about Physician Assistants and Nurse Practitioners
Many older adults are more familiar with a more traditional healthcare model where a primary care doctor administers primary care.
Additionally, older adults seemingly have more preconceived biases and misconceptions that NPs and PAs are less qualified than MDs.
However, these biases do not reflect the reality of modern healthcare.
NPs and PAs undergo rigorous education, including advanced degrees and clinical training, equipping them to effectively diagnose, treat, and manage various health conditions.
Studies quoted above have shown that the care provided by NPs and PAs is comparable to that of physicians, with patient outcomes, satisfaction levels, and safety records all aligning closely with those seen in physician-led care.
By understanding and recognizing the capabilities of NPs and PAs, older adults can embrace a more comprehensive and collaborative healthcare model that leverages the strengths of all healthcare professionals to provide the best possible care.
The Role of Nurse Practitioners and Physician Assistants in Primary Care
Nurse practitioners and physician assistants are crucial in delivering accessible, high-quality healthcare, particularly in primary care settings.
Their rigorous clinical training and unique approach enable them to provide top-notch care.
Comprehensive Diagnostics and Treatment
NPs and PAs can diagnose and manage a broad spectrum of health conditions.
They apply their medical knowledge to effectively treat older adult patients, from acute infections to managing chronic diseases like diabetes or hypertension.
Chronic Condition Management
They excel in monitoring and adjusting treatment plans for chronic conditions, focusing on optimizing health over the long term rather than just treating symptoms.
This involves regular assessments and modifications of medication regimens as needed.
Prescriptive Authority
NPs and PAs can prescribe medications in most states, but the specific regulations and limitations vary by location.
Checking with the state’s licensing board or the healthcare provider’s practice is advisable.
NPs and PAs training in pharmacology ensures they can safely and effectively manage their patients’ medication needs.
Preventive Health Care
They strongly advocate preventive measures, guiding older adult patients to maintain a healthy lifestyle and prevent diseases before they start.
Preventative measures may include vaccinations, screenings, and personalized advice on diet and exercise.
Patient-Centered Approach
Education for both NPs and PAs emphasizes patient-centered care, prioritizing the patients’ emotional, psychological, and physical needs.
These clinicians are trained to listen carefully to patient concerns, making them effective at building trust and facilitating open communication.
Psychosocial Health Management
Understanding the link between psychological well-being and physical health, NPs and PAs assess psychosocial factors that could affect the patient’s health.
This holistic approach ensures comprehensive care that addresses all patient life facets.
By incorporating these professionals into primary care settings, healthcare systems ensure that patients receive well-rounded, effective care that treats illnesses, promotes overall health, and prevents future health issues.
This model of care is particularly beneficial for older adults, who may have more complex health needs and could benefit from the thorough, compassionate approach NPs and PAs take.
Next, we’ll examine nurse practitioners’ specific role in providing primary care to older adults.

What is a Nurse Practitioner?
A nurse practitioner is an advanced practice registered nurse authorized to deliver comprehensive healthcare services.
NPs are held to the same stringent legal and ethical standards as physicians and are deeply committed to offering personalized, high-quality healthcare.
Their dedication extends beyond routine care; nurse practitioners are pivotal in bridging healthcare gaps, ensuring all population segments have access to the care they need.

A Nurse Practitioner’s General Scope of Practice in Primary Care
Nurse practitioners provide essential medical services across a patient’s lifespan, emphasizing health promotion and disease prevention.
NPs offer expertise in various settings – from urban hospitals to rural clinics- whether working independently or collaboratively with physicians.
A nurse practitioner’s scope of practice may include:
- Acute care;
- Family primary care ;
- Gerontological Care;
- Pediatric Care;
- Occupational Health;
- Mental health/Psychiatric.
A General Outline of a Nurse Practitioner’s Healthcare Duties
Nurse practitioners are highly skilled in:
- Conducting thorough physical exams;
- Managing prescription medications;
- Diagnosing and treating numerous medical conditions;
- Ordering and interpreting diagnostic tests;
- Providing counseling and education to individuals and families.
- Carrying out routine healthcare maintenance, such as immunizations and well-child care.

Nurse Practitioners’ Contributions to Public Health
According to the Nurse Practitioner Association of Maryland, there are over 205,000 nurse practitioners nationally, with around 3,500 practicing in Maryland alone.
Nurse practitioners are pivotal in expanding access to healthcare in America, particularly in underserved urban and rural communities like Western Maryland and Maryland’s Eastern Shore.
Their focus on primary care, preventive health, and patient education positions nurse practitioners as crucial healthcare responders, often serving as the first point of contact for many Maryland families.
A Nurse Practitioner’s Prescriptive Authority
Recent legislative changes in many states have enhanced the autonomy of nurse practitioners by granting them full practice authority, thus eliminating the requirement for physician oversight.
According to a study by Markowitz and Smith (2023), using a unique analytical method to assess whether allowing nurse practitioners to practice independently increases the risk of patient harm, as indicated by malpractice payouts and adverse action reports, reveals no evidence of increased harm.
Furthermore, the study’s findings suggest that physicians may experience decreased malpractice claims following these legislative changes.
This track record highlights nurse practitioners’ commitment to safe, effective patient care.

NPs have established themselves as indispensable members of our healthcare community through decades of dedicated service since the role’s inception, beginning in 1965 at the University of Colorado.
A nurse practitioner’s blend of clinical expertise, patient care, and community health support is vital to enhancing the flexibility, responsiveness, and overall efficacy of our American healthcare system.
Maryland Nurse Practitioner Certification Criteria
In Maryland, nurse practitioner certification is a heavily regulated process designed to ensure that all NPs meet the highest standards of professional practice before they begin to provide healthcare services to their patients.
Below are the specific criteria for nurse practitioners to obtain certification in Maryland, set forth by the Maryland Board of Nursing and enshrined in the Maryland COMAR regulations.
Maryland Nurse Practitioner Licensure and Good Standing
An applicant for a Maryland nurse practitioner license must hold a current Maryland license to practice registered nursing or possess a multistate licensure privilege to practice registered nursing, both of which must be in good standing.
Educational Qualifications for Maryland Nurse Practitioners
To obtain certification in Maryland, a nurse practitioner applicant must have graduated from a graduate-level nurse practitioner program accredited and approved by the Maryland Board of Nursing.
This educational program must meet the Board of Nursing’s strict educational criteria, specified at the master’s level or higher.

National Certification for Maryland Nurse Practitioners
- Specialization: The NP applicant must hold current national certification in each area of specialization they wish to practice.
- Certifying Body: This certification must be from the American Academy of Nurse Practitioners Certification Board (AANPNCB) or another national certifying body recognized by the Maryland Board of Nursing.
A Maryland Nurse Practitioner’s Application to Practice
Each NP applicant must submit a completed application to the Maryland Board of Nursing for certification as a nurse practitioner in each area of specialization they seek to practice in.
Compliance with COMAR Requirements
Applicants must comply with all the requirements outlined in Maryland COMAR 10.27.01.04, which details additional nursing practice and conduct standards.
Maryland Nurse Practitioner Language Competency
Nurse practitioner applicants must demonstrate written and oral competency in English.
The Maryland Nurse Practitioner Mentorship Requirement
Suppose the Maryland nurse practitioner applicant has not previously been certified by the Maryland Board of Nursing or any other state Board of Nursing.
In that case, the applicant must identify a designated mentor for 18 months, as defined by Board of Nursing regulations.

Next, I unwind the specific role of physician assistants in primary care.
What is a Physician Assistant?
A physician assistant is an individual licensed to practice medicine under the supervision of a physician, performing delegated medical acts that are:
- Within a supervising physician’s scope of practice;
- Appropriate to the physician assistant’s education, training, and experience; and
- Consistent with the delegation agreement filed with the Maryland Board of Physicians.

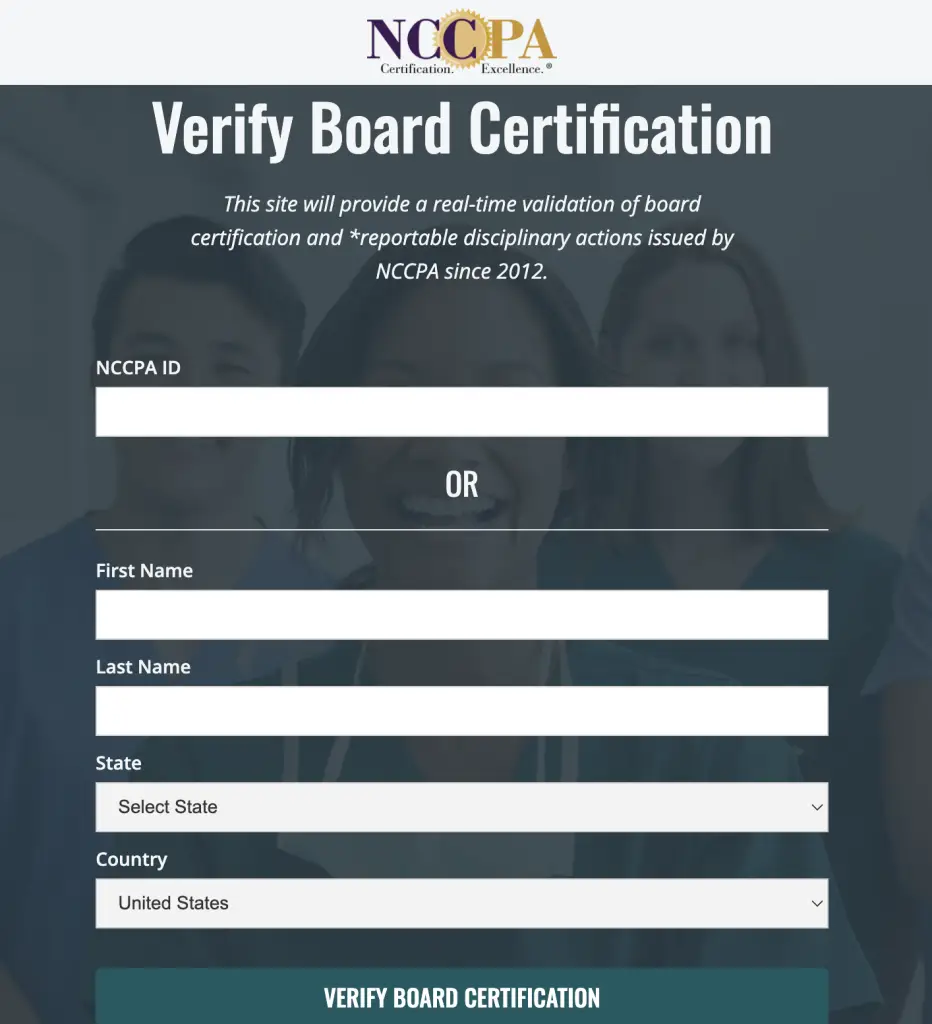
Verify a Maryland Physician Assistant’s Certification with the NCCPA and the Maryland Board of Physicians
Verifying a Maryland physician assistant’s certification is essential to ensure that the PA meets the highest professional standards of knowledge and skills.
The National Commission on Certification of Physician Assistants (NCCPA) is the sole certifying body for PAs in the United States.
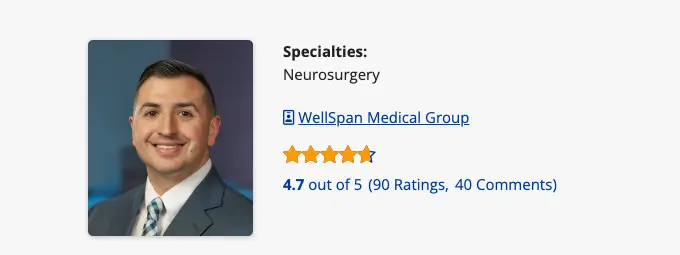
To verify the certification of a Maryland physician assistant, visit the NCCPA’s official certification verification page or click the photograph below.
Please click the image below to visit the official Maryland Board of Physicans website to search for a Maryland physician and physician assistant’s profile.
A Physician Assistant’s Scope of Practice
In primary care, PAs are pivotal in ensuring comprehensive and continuous care, especially for older adults and adults with disabilities.
They address various health issues, from preventive care to complex medical management, thereby enhancing the efficiency and reach of primary care services.
Comprehensive Patient Evaluation
PAs take detailed patient medical histories and review their patient’s medical records to construct thorough medical status reports.
This foundational work is crucial for effective treatment planning.
Physical Examinations
PAs conduct comprehensive physical examinations and meticulously document all relevant patient data to ensure a holistic understanding of their health.
Data Interpretation and Management Plans
PAs interpret medical data critically to determine the best management and treatment plans for their patients, working within the scope and guidelines set by their supervising physicians.
Diagnostic Procedures
PAs are authorized to initiate and perform various diagnostic procedures, helping to pinpoint health issues accurately and expediently.

Patient Education and Care Guidance
Physician assistants provide essential healthcare instructions and guidance to their patients.
Clinical Service Delivery
PAs assist in delivering a variety of medical services in various healthcare settings, including:
- Documenting patient progress;
- Issuing diagnostic and home health orders;
- Executing specific medical orders under the direct supervision of a managing physician.
Prescriptive Authority
Maryland PAs can prescribe and administer medication to their patients, including controlled substances, with delegated authority from a supervising physician.
A PA’s prescriptive authority is vital in managing their older adult patients’ chronic conditions.
Physician Assistants’ Contributions to Public Health
There are over 139,000 physician assistants nationally, with approximately 3,200 practicing in Maryland.
Like nurse practitioners, physician assistants enhance healthcare accessibility, especially in underserved areas such as Western Maryland and Maryland’s Eastern Shore.
Physician assistants are committed to providing comprehensive primary care, managing chronic conditions, and promoting preventative health measures, making them indispensable in public health. They often serve as the initial point of contact for many families, guiding them through the healthcare system with professionalism and care.
Maryland Physician Assistants’ Prescriptive Authority Overview
In Maryland, physician assistants can prescribe medication.
However, a supervising physician must delegate authority to a PA through a formal agreement.
Below is a screenshot of a sample Maryland delegation of services agreement between a practicing physician and a physician assistant, as enumerated in the Health Occupations Article, § 15-302, Annotated Code of Maryland.

What Medications Can Maryland PAs Prescribe?
- Prescription drugs (legend drugs) as defined by the Federal Food, Drug, and Cosmetic Act;
- Controlled dangerous substances (Schedules II-V) with a valid Maryland Controlled Dangerous Substance (MCDS) license and a federal Drug Enforcement Administration (DEA) registration.
However, Maryland PAs cannot prescribe Schedule I controlled dangerous substances (the most restricted category).
Additional Requirements for Maryland PA Prescriptive Authority
PAs practicing in Maryland must meet specific qualifications before receiving prescriptive authority, including:
- Passing the National Commission on Certification of Physician Assistants (NCCPA) exam within the previous two years or completing eight Category I hours of pharmacology education.
- Having a bachelor’s degree or equivalent (120 credit hours) or two years of work experience as a physician assistant.
Maryland Controlled Dangerous Substances
The Maryland Controlled Dangerous Substances Act defines controlled substances by incorporating the federal classification system.
Schedule I Drugs
These have the highest potential for abuse and no currently accepted medical use in treatment.
Examples include (this list is not exhaustive):
- Heroin
- LSD
- Cannabis (although Maryland has legalized recreational cannabis use for adults 21 and over; however, cannabis remains a Schedule I substance federally)
- Ecstasy (MDMA)
- Peyote

Schedule II Drugs
These drugs have a high potential for abuse but also have accepted medical uses.
Examples include (this list is not exhaustive):
- Oxycodone (OxyContin)
- Hydrocodone (Vicodin)
- Fentanyl
- Methamphetamine
- Cocaine

Schedule III Drugs
These drugs have a moderate potential for abuse and have accepted medical uses in treatment.
Examples include (this list is not exhaustive):
- Suboxone (used in opioid addiction treatment)
- Codeine with a low amount (less than equal to 200mg) of another substance
- Ketamine

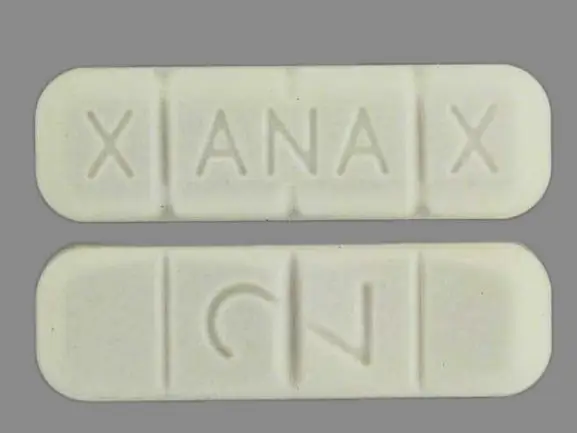
Schedule IV Drugs
These drugs have a low potential for abuse and have accepted medical uses in treatment.
Examples include (this list is not exhaustive):
- Xanax (alprazolam)
- Valium (diazepam)
- Klonopin (clonazepam)
- Modafinil (used for sleep disorders)
Schedule V Drugs
These drugs have the lowest potential for abuse and have accepted medical uses in treatment.
Examples include (this list is not exhaustive):
- Cough syrups with small amounts of codeine
- Imodium (antidiarrheal)
Expanding Physician Assistant Autonomy and Its Impact on Patient Safety and Malpractice Claims
Recent modifications in state laws across the United States, as detailed by the American Academy of PAs (AAPA) on their legislative updates page, have significantly increased physician assistants’ autonomy by expanding their prescriptive authority and reducing the required level of direct physician oversight.
The shift towards greater independence allows PAs to utilize their entire training and expertise more effectively.

A February 2024 study released by the Journal of Medical Regulation indicates that increasing physician assistants’ scope of practice does not compromise patient safety and shows no evidence that greater autonomy for physician assistants leads to increased incidents of patient harm.
While definitive evidence is limited, ongoing research suggests that changes in physician assistant law may not lead to increased malpractice claims.
The safe and effective care provided by physician assistants, as supported by studies on patient outcomes, could potentially contribute to fewer overall malpractice claims in healthcare systems.
The Enduring Impact of Physician Assistants
Since the profession was established in the mid-1960s, following a curriculum developed at Duke University, physician assistants have become essential to our healthcare system.
Their unique combination of medical knowledge, clinical skills, and focus on patient and community health significantly enhances healthcare services’ adaptability, responsiveness, and efficiency.
Physician assistants’ deep clinical expertise and dedication to patient and community welfare are pivotal in fortifying the healthcare system, making it more robust and capable of meeting diverse patient needs across the United States.
Embracing NPs and PAs for Comprehensive, Cost-Effective Primary Care
Nurse practitioners and physician assistants are essential to modern primary care.
They provide high-quality, cost-effective, and patient-centered healthcare, and their rigorous education and collaborative approach significantly enhance patient outcomes, especially for older adults.
Are you ready to embrace nurse practitioners and physician assistants as your future primary care provider?
Ryan Miner, MBA | Co-Founder and Podcast Host | The Senior Soup
Hi, I'm Ryan!
I co-founded The Senior Soup Soup with Raquel Micit in September 2022. Together, we host The Senior Soup Podcast.
I am a community relations manager for Ennoble Care in Maryland, where I am responsible for marketing our home-based primary care healthcare practice.
I have over 15 years experience in healthcare, senior services, senior care, marketing, public policy, and search engine optimization.
I have a MBA from Mount St. Mary's University and a BA from Duquesne University.
- Ryan Miner